PharmD Careers



Our graduates go on to work in a wide range of practice settings including hospital pharmacy, community pharmacy, research and drug development, pharmacoeconomics, managed care, nuclear pharmacy, home health care, government agencies, and academia.
By the Numbers
88%
of graduates receive first/second choice position
No. 1
residency match rate in the U.S.
94%
NAPLEX pass rate
last updated on Jun. 21, 2022
| Graduating Year | Four-Year Graduation Rate (%) | Delayed (%)* | Dismissed (%) | Withdrew (%) |
|---|---|---|---|---|
| 2023 | 97 | <7 | 0 | <2 |
| 2022 | 93 | <8 | 0 | <1 |
| 2021 | 97 | 3 | 0 | <1 |
| 2020 | 94 | <4 | <1 | <1 |
| 2019 | 90 | 8 | 0 | 2 |
| 2018 | 96 | 2 | 0 | 2 |
| 2017 | 97 | 3 | <1 | 0 |
| 2016 | 96 | 2 | 0 | 2 |
| 2015 | 93 | 4 | 0 | 2 |
| 2014 | 92 | 5 | 3 | 1 |
| 2013 | 95 | 3 | <1 | <1 |
| 2012 | 92 | 3 | <1 | 4 |
| 2011 | 90 | 5 | 4 | <1 |
| 2010 | 95 | 2 | 0 | 3 |
| 2009 | 94 | 3 | 1 | 2 |
| 2008 | 97 | 2 | <1 | <1 |
2023: 11 students were delayed: 4 to meet the requirements for the PharmD/MBA dual degree program, 3 to meet the requirements for the PharmD/MPH dual degree program, 2 for leave of absence, 1 for medical leave, and 1 other
2022: 11 students were delayed: 5 to meet the requirements for the PharmD/MBA dual degree program, 2 to meet the requirements for the PharmD/MPH dual degree program, 2 for leave of absence, 1 for medical leave, and 1 other
2021: 5 students were delayed: 2 to meet the requirements for the PharmD/MBA dual degree program, 2 for academic reasons, and 1 medical leave
2020: 6 students were delayed: 4 to meet the requirements for the PharrmD/MPH dual degree program, 1 to meet the requirements for the PharrmD/MBA dual degree program, 1 for medical reasons
2019: 13 students were delayed: 3 to meet the requirements for the PharrmD/MPH dual degree program, 1 to meet the requirements for the PharrmD/MBA dual degree program, 2 for academic reasons, 3 for medical reasons, 3 for leave of absence, and 1 other
2018: 4 students were delayed: 3 for medical reasons and 1 to meet the requirements of the PharmD/MPH dual degree program
2017: 8 students were delayed: 3 for academic reasons, 1 for medical reasons, 3 to meet the requirements of the PharmD/MPH dual degree program, and 1 to meet the requirements of the PharmD/MBA dual degree program
2016: 4 students were delayed: 1 for academic reasons, 2 for medical reasons, and 1 for other reason
2015: 7 students were delayed: 4 for academic reasons, 1 for medical reasons, and 2 for other reasons
2014: 7 students were delayed: 2 for academic reasons, 4 for medical reasons, and 1 to meet the requirements of the PharmD/MBA dual degree program
2013: 5 students were delayed: 3 for academic reasons, 1 for medical reasons, and 1 to meet the requirements of the PharmD/MBA dual degree program
2012: 5 students were delayed: 1 for academic reasons, 3 for medical reasons, and 1 to meet the requirements of the PharmD/MBA dual degree program
2011: 7 students were delayed: 5 for medical reasons, 2 for other reasons
2010: 4 students were delayed: 1 for academic reasons, 2 for medical reasons, and 1 for other reasons
2009: 4 students were delayed: 3 for academic reasons, 1 for other reason
2008: 2 students were delayed: 1 for academic reasons, 1 for medical reasons
as of Jan. 26, 2024
| Graduating Year | NAPLEX First-Time (%) | National Benchmark (%) | UNC Performance vs. National |
|---|---|---|---|
| 2023 | 93 | 79 | 14% Higher |
| 2022 | 93 | 78 | 15% Higher |
| 2021* | 96 | 82 | 14% Higher |
| 2020 | 98 | 86 | 12% Higher |
| 2019 | 92 | 87 | 5% Higher |
| 2018 | 95 | 89 | 6% Higher |
| 2017 | 92 | 88 | 4% Higher |
| 2016 | 95 | 86 | 10% Higher |
*revised NAPLEX blueprint
as of Jan. 26, 2024
| Graduating Year | MPJE In-state First-Time (%) | National Benchmark (%) | UNC Performance vs. National |
|---|---|---|---|
| 2023 | 92 | 74 | 18% Higher |
| 2022 | 93 | 76 | 17% Higher |
| 2021 | 89 | 79 | 10% Higher |
| 2020 | 94 | 83 | 11% Higher |
| 2019 | 92 | 83 | 9% Higher |
| 2018 | 93 | 84 | 9% Higher |
| 2017 | 90 | N/A | N/A |
| 2016 | 95 | N/A | N/A |
as of Nov. 1, 2023
| Graduating Class Year | Total Graduates (1) | Position Acceptance Rate (2) | Residency (3) | Fellowship (4) | Employment (5) | Other (6) | Lost to Follow-Up (7) | North Carolina Position (8) |
|---|---|---|---|---|---|---|---|---|
| 2023 | 155 | 148 (95%) | 80 (52%) | 23 (15%) | 42 (27%) | 3 (1%) | 7 (5%) | 51 (33%) |
| 2022 | 135 | 124 (92%) | 80 (59%) | 14 (10%) | 29 (21%) | 1 (1%) | 11 (8%) | 46 (34%) |
(1) Total number of students that graduated in May of the same graduating class year.
(2) The Position Acceptance Rate is the total amount of students that have accepted a position by November 1st divided by the total amount of students that graduated in May of the same graduating class year.
(3) Residency is defined as accepting a post graduate residency training position in any of the following specialties. Acute Care, Ambulatory Care, Community, Hospital/Health System Admin, Managed Care or Other.
(4) Fellowship is defined as accepting a post graduate fellowship training position in any of the following specialties. Medical Affairs/Medical Information/Medical Communications, Clinical Research/Drug Development, Regulatory Affairs, Managed Care, Health Economics & Outcomes Research/Market Access, Drug Information, Commercial, Clinical Pharmacology/Pharmacokinetics/Pharmacodynamics/Pharmacometrics.
(5) Employment is defined as accepting a position in Community Pharmacy (chain), Community Pharmacy (independent), Nuclear, Life Sciences Consulting, Long Term Care, Consulting or Other.
(6) Other is defined as any position accepted that is not categorized as employment, residency or fellowship. In some cases, this might be enrollment in postgraduate education.
(7) A student is considered lost to follow-up if our Career Service offices has not documented the position choice of the student by November 1st of the graduating year.
(8) A student is reported as in North Carolina if we have data that indicates their physical work location city and state. Note – If the employer is in another state and the student is working remotely in North Carolina, then we consider this a North Carolina placement.
2022 data collected via the Graduating Student Survey that closed on 5/2022. This was supplemented with student follow-up through November. Please click HERE to view the summary results.
2021 data collected via the Graduating Student Survey that closed on 5/2021. This was supplemented with student follow-up that ended in November. Please click HERE to view the summary results.
2020 data collected via the Graduating Student Survey that closed on 5/2020. This was supplemented with student follow-up that ended in November. Please click HERE to view the summary results.
2019 data collected via the Graduating Student Survey that closed on 5/2019. This was supplemented with student follow-up that ended in November. Please click HERE to view the summary results.
Authoritative Data Source – Report Catalog
Alumni Spotlight
The Profession of Pharmacy
Hear From Our Alumni
More From Our Alumni
Meet alum DeLon Canterbury, President and Chief Executive Officer at GeriatRx, Inc.

DeLon Canterbury, Pharm.D., BCGP, (Class of ’14), is President and Chief Executive Officer of GeriatRx, Inc. in Durham, N.C., and is a Certified Community Pharmacogenomics (PGx) Consultant. Canterbury has dedicated his career to serving low income and rural socioeconomic populations across the Triangle, aiming to give his patients healthier lives by supporting them in their health journeys.
Please describe your practice setting. What makes your career path unique?
I work as a consultant pharmacist at GeriatRx, which uses a patient-centered approach to holistic care. We implement telehealth, Comprehensive Medication Management and Pharmacogenomics to provide cost-effective solutions for patients. GeriatRx provides invaluable health care consulting services and demonstrates the unique skillset pharmacists have in improving health care outcomes while managing our patients effectively with precision medicine and evidence-based Practices. GeriatRx deprescribes unnecessarily written medications and we work to reduce costs for our patients while removing the side effect headache from our patients’ providers. Our job is to find complex solutions to really complex health barriers for our patients, such as assessing the social determinants of health (food, shelter, community resources, health education) that are linked to positive health outcomes. It’s about the interdisciplinary team-based approach to care that health care needs.
What led you to this career path? What steps did you take?
It’s kind of two stories in one. I’ll start with the very real, raw side. I was a retail pharmacy manager for about six years. I just kept seeing the very same patients who were either minorities or elderly coming in with the same medication errors. It ended up being such a theme that I thought, ‘how can we avoid this all together? How can we stop them from coming in with duplicate therapies and drug interactions that are causing harm?’ Time and time again, I saw the same issues. And you think, ‘this is broken. Health care is broken.’ It struck a chord with me to have to tell patients their co-pay was $1,200, even after I checked the coupons four times and did everything I could. Their heart is breaking, my heart is breaking. I felt like I wasn’t truly helping people. That led me down a dark road of depression and unfulfillment in pharmacy. I felt like I was a part of the problem and I was another cog in the wheel. So, I tried to pull myself out of this depression by remembering why I got into pharmacy in the first place, which was for community service. It started with volunteerism. So I found an amazing group – Senior Pharmacists, led by Gina Upchurch who’s also a Tar Heel alum. She runs a nonprofit called Senior PharmAssist that focuses on helping older patients with Medicare assistance and Medicare enrollment in Durham. I started working on their formulary committee and started researching medications we should put on or take off the formulary, and that was so fun! It got my fire back; it got my passion back. We were able to give that extra help outside of the four walls of a pharmacy and it encouraged me to see how pharmacists can tremendously influence the way health care is delivered and change the impact with have.
Story number two, my grandmother suffered from dementia in her later years, and that encouraged me to get that Board Certified Geriatrics Pharmacotherapy Certificate. We had to move her from New York to Atlanta because she was declining so poorly in her care and her dementia was worsening. Come to find out, when we went to refill her prescriptions, a pharmacist realized she was on an inappropriate medication that was worsening all of her symptoms. Preventable. My parents suffered for months in trying to figure out the cause, with countless medical bills and expenses wasted on a condition that was due to an inappropriately prescribed medication. Imagine how many other caregivers and family members are suffering just like this without a pharmacist to guide them along their medication management journey? Her side effects completely subsided after the pharmacist talked to her doctor and changed her medication. Health care shouldn’t be so plug and chug that those errors slip through the cracks. That also inspired me to continue in pharmacy, but to also specialize in geriatric care.
What does a typical workday look like for you?
Day-to-day, I’m following up with providers as well as patients to make sure we are keeping up with patients’ health care goals. For patients, I’m checking in to make sure they are keeping up with their goals, asking questions such as, “are we checking our blood sugar and blood pressure every day?”
Each day varies based on patient needs. Some days are about motivational interviewing and talking about medication adherence and compliance. Some days we are talking about financial barriers to be able to adhere to those medications. Other days, we are talking about new therapies and pharmacogenomics, or health literacy.
We are able to do assessments and customize patient needs like falls risks, or anticholinergic toxicity burden. We look at the social determinants of health that impact health outcomes for our patients while providing medication/therapy management and pharmacogenomic testing if needed.
With us, you’re getting a full medication/therapy review. We provide that record to patients and their provider(s). Once a patient comes on board, we also go through each disease state they have and educate on each disease. We are teaching our patients everything we can about their body as if we are presenting a patient case from pharmacy school in a fun and easy to follow manner. We’re educating and empowering our patients. With education we hope comes change in behavior.
And when we communicate with the patient, we also consult their doctor and identify any barriers that we can address as a team. Everything is team-based and patient-centered for us. This is why we stress the need for a holistic and public health approach model to care.
We serve a mixed demographic of patients. So right now, during COVID-19, the majority are skeptical of the vaccine. But they know they can reach out to us at any time and ask their questions. I make myself readily available for anything COVID because of the misinformation. That’s been at the forefront of our practice. I’m offering free consultations to our patients, and to anyone who has questions about the vaccine. It’s led to me being in town halls, speaking on church panels, being a part of media interviews, and being hosted on several news channels and radio features which has given us much traction. I’m on the Executive Board of the African American COVID Task Force (AACT+) here in Durham and it’s been amazing because we’ve helped to provide testing, resources and community connections so people can get the support they need in these tough times. We’re here to educate and advocate so our patients make the best decisions. Through media interviews, I’ve also been able to speak to some of the power pharmacists can really have in this time of need and figuring out vaccine logistics. I’ve also been able to address COVID-19 and systemic racism that’s in play and the lack of equity we are seeing in the vaccine rollout across the state. At the time, 8 or 9 percent of African Americans had gotten the first dose and 80 percent were white. It speaks to the fact that systemic racism, or medical racism, has always been there, but COVID has now shed a mirror to the gaps in health care especially within our Black communities.
Describe the most exciting or rewarding aspect of your role?
On a day to day, I leave every speaking engagement knowing someone has peace of mind. Each day, there are people who leave understanding and trusting the science is there. That’s especially important for me as a Black pharmacist. That barrier still hits home today. We still have the blemish of the Tuskegee experiment fresh in our minds. We still have the North Carolina eugenics program fresh in our minds that sterilized black females for population control, funded by our state government. So with the COVID-19 vaccine, there’s a need to address that hesitation. And when you start hearing it from your own family members, you think ‘ok, I’ve got to do something. I’ve got to speak up.’ I can’t let my loved ones who are high risk just play the misinformation game. We must never downplay the history and ugliness of the medical past towards people of color, but we cannot conflate half-truths in the midst of a global pandemic where Black, Latino, and Indigenous people are dying at rates 2-4 times more than white Americans.
Describe the most fulfilling moment of your career?
Honestly, one of my most fulfilling moments was working with an 80-year-old patient. The poor thing was prescribed 36 medications. Completely ridiculous. I’m seeing she’s on five different drugs that will contribute to anticholinergic toxicity, she’s on two other sleep meds. Her caregiver described her as a “walking zombie.” She’s was barely responsive, she was depressed, she was dying. After we reviewed her case and managed her meds, we were able to reduce her down to 8 medications, which was amazing. If it wasn’t for our Comprehensive Medication Management, this patient would have been thrown into a nursing home costing over $150,000 annually. As a consultant pharmacist, GeriatRx was asked to serve as a medical expert on this case and provide the evidence behind our pharmacy interventions. I stated in court that it’s not her, it’s the medications. We were able to save her family hundreds of thousands of dollars, because her family was battling to seize all of her assets, including her home, independence, and access to grandchildren. GeriatRx not only worked with her provider on developing an efficient deprescribing plan but we were able to get our patient her life back. She got back to normal. That was the most humbling and rewarding moment in my career as a pharmacist and that solidified my calling and purpose to advocating and empowering my patients against a broken health care system.
Describe the most challenging aspect of your role?
Some people are still new to the idea that pharmacists can even do consulting work. It’s a relatively minor barrier when you share the great stories GeriatRx has accomplished, but patients may be hesitant. The traditional lens of how people look at pharmacists is something we need to change, as its outdated and ineffective. Pharmacists have to be loud and be our own champions in demonstrating our invaluable services to the health care team. People don’t know much about pharmacogenomics, but pharmacists are leading this charge, which is another service GeriatRx includes with our Comprehensive Medication Management.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
You’ve got to get exposed to know what you’re getting into. Joining a pharmacist association has been extremely beneficial for me such as the Student National Pharmaceutical Association and American Society of Consultant Pharmacists. Join the ones that speak to you. Build relationships with your faculty and staff. If you really wanted to break out of the traditional roles, find mentors in untraditional roles. Follow people that are entrepreneurs within the pharmacy space and gain the tools to be your own entrepreneur. Go to conferences and network. Networking has been so valuable. And invest in yourself with coaching or conferences.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
It’s really the ones who think out of the box that are going to do well. And remember to go into pharmacy from a place of passion and a place of servitude. Don’t do it for the money or the prestige. Do this because you know someone else is going to benefit from your education. If you are considering pharmacy, go volunteer in a pharmacy. Get into the hospitals. Start from the ground up. And if you don’t know where to start, start with your teachers because they can guide you. I was extremely fearful to ask for support or letters of recommendation. You don’t learn or realize that until you’re out of school. Traditional pharmacy is not very pretty right now, so don’t feel confined. Show up. Think outside of the box.
Meet alumus Franklin Roye, Pharm.D., President of IndyCare

In this alum spotlight, we chat with Franklin Roye, Pharm.D. (Class of ’03), President of IndyCare, a retail health and wellness center based in the Triangle that provides technology-enhanced, collaborative care on-demand, at your local independent community pharmacy. IndyCare works to transform independent pharmacies into integrated healthcare hubs that empower local communities to thrive through exceptional health.
Please describe your practice setting. What makes your career path unique?
Right now, I work at IndyCare and I am one of the co-founders of the company. It’s a community pharmacy health hub practice setting. We have an independent community pharmacy and an embedded medical clinic where our pharmacists and our medical providers work collaboratively together to deliver simplified, high quality care for patients. The collaborative aspect of this is what I think makes it unique.
There are certainly retail pharmacies out there with clinics inside of them, think CVS minute clinic, Walgreens, Kroger. However, what you find at these places is they see patients in a clinic space that’s within the pharmacy, but they don’t actually involve the pharmacist or the pharmacy staff in care delivery. We felt that was a real wasted opportunity, given that patients see their pharmacists five to 10 times more often than their medical provider. So we created this true collaborative care model of community pharmacy where our pharmacists can turn those frequent encounters into engagements where they provide patient care and get financially compensated for that.
What led you to this career path? What steps did you take?
It definitely wasn’t a preconceived plan and that brought me here. I worked most of my career in the biopharmaceutical industry in various commercial roles, such as sales, marketing account management, strategic consulting and business development.
I started out with GlaxoSmithKline here in North Carolina and went with them to New York City after that. Next, I took an international opportunity with a market access consulting firm called the NUCLEUS Group. That took me to Singapore, where led their business development team for the Asia Pacific region, covering a region spanning from China to Australia and everything in between. Eventually I shifted again to a similar role in Asia with PPD, a global contract research organization. Three years ago, I came back to the US to start IndyCare with a pharmacy school friend of mine Greg Vassie. So this is really my first foray into frontline healthcare.
What does a typical workday look like for you?
It’s pretty intense. I start my day at five o’clock in the morning so I can get up, get a coffee, get a little exercise in and have some time to think through my plans before my kids get up. Then, I’m onsite at the clinic and pharmacy about three days a week, working on operations that include managing our employees, providing training, rolling out new services and doiong some overall problem solving. I usually also have a few virtual meetings each day with different partners and vendors that we work with. Those cover everything from marketing, technology platforms that we use, insurance companies and other collaborators. We’re constantly seeking new information because the consumer health care industry is fast paced and constantly evolving. The other days of the week that I’m not at the clinic, I’m working more on medium-to-long-term growth initiatives for the company. Looking at new services that we want to implement, evaluating different business partners and business development.
Describe the most exciting or rewarding aspect of your role?
Right now, for me, it’s definitely the feedback that we get from patients. The feedback that we’ve gotten from patients has really blown away even our own high expectations, and I think that’s when you really feel like you’re making an impact.
Describe the most challenging aspect of your role?
The US healthcare system is not easy to disrupt. You can have a very simple and common-sense approach to providing what patients, pharmacists and medical providers want, but theirs is a complex maze of legal, regulatory, financial, and insurance requirements that may be a barrier to your plan. You have to work incredibly hard to figure out how to navigate this complex matrix of stakeholders and still deliver on your plan and that’s a constant challenge.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
I believe it’s very important to study the business of health care and trends in healthcare consumerism. In pharmacy school, you devote most of your learning to the science and the clinical aspects of our profession, which is a critical foundation. However, once you start working, things shift pretty dramatically, and the clinical side often is a much smaller part of what you do every day. A large part of what you do is navigating non-clinical business information and solving real world business problems, so learning about the business of health care and healthcare consumerism will provide a good knowledge base to work in a setting like ours.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
Take advantage of every opportunity, both within and outside pharmacy school to supplement your clinical education. When I was at the School of Pharmacy, I took electives at the business school, for example. Also, learn about big data and start to develop a baseline level of data fluency. Being able to look at, understand and act upon data is going to be a significant part of your professional life going forward. Lastly, get as much diverse experience as you can. You’re going to get plenty of clinical training through the School and through your rotations, so it’s always going to be helpful to mix that with other types of business experience.
What advice would you give to a high school student?
Really look into trends in the profession because pharmacy is changing very rapidly and by the time you get out of pharmacy school, it may not be what you think it is now. Pharmacy is a very valuable education and training. The medical and pharmaceutical knowledge you gain from a pharmacy program can serve you well in a number of different career paths, so I would say keep an open mind as to what a pharmacist career means. There are trends in our industry with automation and technology that will lead to a contraction of traditional dispensing pharmacy roles which is what many people outside of the profession think of first. However, for every loss there are also gains in areas of healthcare that people may not realize and where your Pharmacy education will allow you to excel professionally.
Can you share a brief story about a time you had a positive impact on patient population or community in your role?
In our practice setting, we have all the ingredients that you need to solve problems for patients. We have pharmacists, medical providers, electronic health record system, contracts with insurance companies and more. When you have all these resources and your small and nimble it gets very interesting as you can find lots of ways to help people because you’re not constrained.
Recently, we were contacted by a gentleman who was desperately searching for help to get his elderly, disabled, homebound mother with Alzheimer’s tested at her home for COVID. He had already checked with the big health systems around the area and several other medical facilities and no one was willing to do it, primarily because they didn’t have a protocol or a policy to do that. He was exasperated and when he came to us and asked if we could help, our response was, ‘sure, why not?!’ There’s nothing stopping us from doing it, we have all the things we need to help this person so why would we not do it. To me that is rewarding because occasionally it can be so simple to solve challenging problems for people if you’re willing to just take the tools you have and use them, without the usual constraints that sometimes prevent our healthcare system from reaching the people who need it the most.
Meet alumna Irene Ulrich, clinical pharmacist at MAHEC

In this alum spotlight, we chat with Irene Park Ulrich, Pharm.D., BCACP, clinical pharmacist in the Mountain Area Heath Education Center’s Department of Family Medicine, and associate professor of clinical education at the UNC Eshelman School of Pharmacy.
Please describe your novel practice setting. What makes your career path unique?
MAHEC is a multidisciplinary health care institution in Western North Carolina. I work in the Family Medicine Department and practice at 2 of the MAHEC satellite practices alongside family medicine physicians. I practice under a collaborative practice agreement, and have my clinical pharmacist practitioner (CPP) designation in North Carolina. In both my practice sites, I have developed a co-visit patient care model in which I see patients in real time alongside the provider, which has been shown to have financial benefit for the practice.
I am also adjunct faculty with the UNC Eshelman School of Pharmacy and precept 8-10 fourth year pharmacy students each year.
My career path is unique is because I started pharmacy school with no intentions of pursuing residency. I felt sure that I would go into community pharmacy and was comfortable with that. However, as I learned more about clinical pharmacy, I began to consider pursuing community pharmacy residency. It was not until I completed by ambulatory care rotation during my fourth year of pharmacy school that it became clear to me that was the path I wanted to take. I decided in the fall of my PY4 year to pursue ambulatory care PGY1 residencies. I was very fortunate to match with Mission/MAHEC in 2012, and ultimately was able to stay on at MAHEC.
What led you to this career path? What steps did you take?
My ambulatory care clinical rotation in the fall of my PY4 year convinced me that this was the route I wanted to take. This rotation was in a diabetes clinic, and I loved that in the process of gathering information for clinical decision making, I would have to learn about the patient’s lifestyle and values. I loved being able to focus on the patient in front of me. I also loved practicing under a CPP where I could make adjustments to medications right then, rather than having to draft a recommendation that may or may not be taken.
Following this rotation, I requested a change in my rotation schedule that would allow me to have one more ambulatory care rotation before ASHP Midyear Clinical Meeting. This solidified my interest in ambulatory care.
What does a typical workday look like for you?
I typically have clinic for at least half of the day. Pre-COVID, I would arrive in clinic and huddle with my physician partners and clinical staff to talk about patients for the day. We would see patients together or sequentially and share documentation responsibilities. If clinic is light, I respond to drug information and med access questions that come to my inbox, or make follow-up phone calls as needed to patients. I also help with insurance communications re: medication recommendations for patients. The other half of the day is often administrative time. In this time, I work on a variety of tasks including but not limited to teaching time with students and residents, scholarly activity including manuscript writing, other initiatives including transgender care work.
Describe the most exciting or rewarding aspect of your (novel) practice role?
Working so closely with my physician colleagues who value and respect my role as a pharmacist is the best aspect. I also love my institution because I have the ability to take on and champion issues that are important not only to me but to our community. The best example of this is my work leading a transgender equity work group that includes representation across our entire organization.
Describe the most challenging aspect of your role?
It is very easy to overcommit. Because anyone can take on new initiatives that they are passionate about, there is often a lot to get involved in.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
There are wonderful resources about ambulatory care practice from large pharmacy organizations including ASHP and APhA.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
Shadow a pharmacist in this setting. The bulk of the work is in face-to-face patient encounters. Those who are excited and energized by this would do well in ambulatory care.
What general advice would you give to a high school or college student who is interested in pursuing a pharmacy career?
Shadowing is so important to understanding what this might look like as a career. No matter how detailed a description, nothing can prepare you more than an in person shadowing experience.
Can you share a brief story about a time you had a positive impact on a patient, population, or community in your role as a pharmacist.
Within the first few weeks of starting at one of my satellite clinic sites, I saw a patient with diabetes who had just obtained private insurance and was referred to me to help her switch from 70/30 insulin to a basal-bolus regimen. We discussed the patterns of her blood sugars, and her desire to lose weight. Based on our discussion, we decided to change to a long-acting insulin analogue and rather than doing bolus insulin, we started a GLP-1 agonist. On follow-up 1 month later, she had lost quite a bit of weight, had not had any low blood sugars and her A1c had gone from 8.5 to 6.5. I continued to check on her in the following years and she lost a total of 30 lbs and her A1c remained in the 6s without requiring any additional changes to her diabetes medications!
Meet alumna Jai Patel

Jai Patel, Pharm.D., BCOP, CPP, (Class of ’11) is the Chair of Cancer Pharmacology & Pharmacogenomics at Levine Cancer Institute in Charlotte, North Carolina.
Please describe your novel practice setting. What makes your career path unique?
My current position at Levine Cancer Institute is Chair of our Department of Cancer Pharmacology & Pharmacogenomics, as well as associate professor in our division of Hematology Oncology. Originally, I was hired at Levine in 2013 as Chief of Pharmacology Research and was promoted to chair of the department in early 2020. My practice setting is a bit novel in that it’s primarily focused on investigator-initiated research, meaning research that we propose, develop, and execute. Most of the research that we do is with pharmacogenomics, so looking at the genetic basis for drug response and drug toxicity. That’s really been an area over the last decade that has been expanding a lot with regards to precision medicine research and looking at clinical implementation of pharmacogenomics testing to improve medication management.
What led you to this career path? What steps did you take?
I think one of the key things for me early on was identifying a champion, a mentor who could help guide me and reflect what I see myself doing. I found that early on in pharmacy school and worked to establish an oncology pharmacogenomics fellowship at UNC. The pharmacogenomics fellowship wasn’t available, but I approached my mentor and said, ‘this is what I want to practice. I have the ambition and drive.’ I had to convince him I was a good investment. Just because something doesn’t exist, doesn’t mean it isn’t possible. That’s what will set you apart from others when trying to build something new. Health care is always changing. Position yourself to be in the forefront of medicine.
What does a typical workday look like for you?
I do have a lot of meetings. I spend a lot more time in meetings than most other pharmacists just because of the nature of research, it’s so collaborative. I work with so many pharmacists, but also physicians, scientists, statisticians, protocol coordinators, and data managers as well. We’ve got a lot of meetings scheduled every day to keep things moving forward. Otherwise, there’s time for data analysis, data collection for studies, manuscript writing, and grant writing – I have to do a lot of scientific writing. I also read a lot of literature, it’s the first thing I do every morning when I get in and I try to get in before others for some ‘quite time’ before things really start to get crazy, so around 6:30 to 6:45 a.m. Being in research, things are always changing and you’re always looking for ways to fill a gap in the literature or improve on how medicine is being practiced. Especially within oncology, there’s just such a vast amount of information and I’m constantly learning every single day, so I read a lot to help me generate new ideas for research. And then there are the presentations and conferences, and I take about five or six students per year on rotation. I do about 50 percent research, 25 percent direct patient care, 15 percent teaching and 10 percent administrative.
Describe the most exciting or rewarding aspect of your (novel) practice role?
The most rewarding is really being able to make that positive impact on patient care, whether that’s directly or indirectly, including pharmacogenomics testing or helping to manage cancer-related symptoms through my clinic time in palliative medicine, or just simply talking to patients. To spend time with the patient and just talk to them about not only their treatment, but also about what’s going on outside of cancer care, including their family or friends or traveling, etc. It’s also really rewarding when we’ve made progress in cancer research that directly benefits patients, which is the whole reason that I got into this field. Selfishly, it’s also really fun to present your research findings at conferences and publish in peer-reviewed journals.
Describe the most challenging aspect of your role?
I think the most challenging aspect, I was put into this role fairly early in my career. I graduated in 2011 and finished my fellowship in 2013, then immediately started here. Levine was a brand-new cancer institute at that time and the building had been up for one year. They were really trying to figure out how they wanted to expand and how they wanted to build this brand-new cancer institute, and they knew they wanted to have pharmacogenomics and pharmacology research to be a part of that. But it was a lot of pressure to figure out how to build a pharmacogenomics and pharmacology research program pretty soon after my fellowship training. I had some great colleagues and mentors that helped along the way.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
Luckily, there is a lot more information out there regarding pharmacogenomics programs than there was 10 years ago. One piece of advice for other folks looking to find a similar opportunity is to look out there on social media like LinkedIn. Connect with folks that have positions within pharmacogenomics or are doing pharmacogenomics and reach out to them see if they can spare 15 to 30 minutes to share with you what they do and why they do it. The best way to learn is to network and connect with people who are already doing what you’re interested in and who can help you achieve what you’re most passionate about.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
Start networking early. I can’t say enough about how important networking is. I wouldn’t be here today without it. Students can shadow professionals, interview professors and professionals. Because I was interested in oncology, I shadowed my oncology professor. Then I developed an interest in pharmacogenomics, so I sought out a pharmacogenomics rotation and ultimately convinced the preceptors to take me as a fellow after graduation.
What general advice would you give to a high school or college student who is interested in pursuing a pharmacy career?
When I was in high school, I worked in retail pharmacy. I knew as a freshman in college that I wanted to be a retail pharmacist. But halfway through pharmacy school I realized all of the other opportunities for pharmacists, whether that be in retail, clinical, regulatory, or research. High schoolers now a days have an advantage with social media to reach out and develop their own interests, seek advice or input from professionals. There are so many people out there who want to help, you just have to take that leap of faith. You don’t have to know exactly what you want to do when you grow up. This is the time of your life where you should be learning about various opportunities and find what excites you.
Can you share a brief story about a time you had a positive impact on a patient, population, or community in your role as a pharmacist?
I’ll talk about implementing pharmacogenetic testing. When I started here at Levine there was no pharmacogenetic testing being done here. We set up a collaboration with our genomics lab which was already established. They had never done pharmacogenomics testing before, but they had done genetic testing for other areas. So, it took a while to set up the infrastructure to be able to build new assays and tests that we could look at specific genes for specific drugs. We then identified where there were opportunities to implement testing. The first test we performed was for an antifungal drug that we use routinely after patients undergo a stem cell transplant. Based off of literature, we knew that there was genetically a third of the population that rapidly metabolized this drug, so they were still at risk of developing a fungal infection. So, we developed an assay to be able to test for that particular gene to identify who would be expected to genetically metabolize this drug very quickly. And we wanted to know that up front before we actually started the drug. We quickly saw that we were able to kind of normalize drug exposure and ensure that all patients were receiving the appropriate dose based off of their genetics. It’s great in that I think we’ve been able to do 700-800 transplants, and we’ve prevented serious fungal infections.
Meet alumna Kimberley Brown, National Field Director of Janssen Infectious Diseases & Vaccines

In this alum spotlight, we chat with Kimberley Brown, Pharm.D. (Class of ’03), National Field Director for Janssen Infectious Diseases & Vaccines. In this role, she leads the development of medical strategy for field-based medical teams and oversees development for the broader organization.
Please describe your novel practice setting. What makes your career path unique?
I have been in the pharmaceutical industry since 2007 and have been in various roles involving medical affairs and research and development.
I joined the Janssen Pharmaceutical Companies of Johnson & Johnson in 2007 as a Medical Science Liaison from the Rainbow Center for Women, Children and Families in Jacksonville, Florida where I served as an HIV Clinical Specialist and Clinical Assistant Professor at the University of Florida School of Pharmacy.
Prior to my current role, I served as Scientific Director for Janssen Research and Development, leading two large Phase III trials and several Phase I studies. From 2015 through Jan 2018, I served as the U.S. Medical Director for the HIV franchise. Before that, I served as Associate Medical Director of U.S. Medical Affairs, Infectious Diseases, where I worked on both the HCV and HIV clinical teams, leading efforts on research trials, as well as product launch activities. I was also the company’s Pharmacovigilance Officer and served as Associate Director of Training with responsibilities for the Virology Medical Science Liaison team.
What led you to this career path? What steps did you take?
I was the nerdy kid who wanted a microscope for Christmas. When I was 10, I remember Dr. David Ho was the Times Man of the Year for discovering AZT, and I was just fascinated by it. For me, studying HIV and hepatitis was the perfect combination of my interests in internal medicine and infectious disease.
From there, my infectious diseases clinical rotation at Moses Cone really set my infectious diseases career in motion – notably, my time at the HIV clinic. I saw that most people coming into the HIV clinic looked like me and were my age at the time. That formulated my ‘why.’ We were seeing huge health disparities, and lack of access to care. Since then, we’ve seen the HIV epidemic continue, but treatment has evolved. Back then, we were trying to keep people alive, now we’ve moved on to more novel therapies to manage this chronic disease.
What does a typical workday look like for you?
Right now, during COVID-19, there’s a lot of focus on medical strategy and building teams. We’re in the process of hiring a new Medical Science Liaison vaccines team that will focus on providing medical information about our vaccines portfolio, driving innovation. Our community liaison team will educate and impact how we can connect to communities. I am spending a lot of time strategizing, collaborating and driving innovation.
Describe the most exciting or rewarding aspect of your (novel) practice role?
Over my career, the most impactful thing was leading an HIV pregnancy study. It gave pregnant women an option to manage their HIV that has proven to be safe and effective (especially in patients with multi-class resistance. Further, these data showed no mother to child transmission which has impacted lives around the world.
My previous roles have been focused on data and research, however my current role has posed a new and interesting challenge – developing leaders that are subject matter experts and strategic.
Describe the most challenging aspect of your role?
Part of the most challenging portion is balancing the needs of health care providers in the community with the business.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
I would encourage those interested in a similar role to reach out to those in the pharmaceutical industry. Take advantage of any internships or experiential opportunities. Call us, network with us, shadow us.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
Express your interest early and often. Take on projects that seem interesting as well as those that don’t. Each experience will allow you to build your skillset and your network.
What general advice would you give to a high school or college student who is interested in pursuing a pharmacy career?
Make sure that you’re prepared by speaking with folks in the profession and have a true understanding of the various realms of pharmacy. Don’t underestimate your potential. And when faced with challenges or closed doors, keep top of mind ‘why not me?’ Continue moving one step forward at a time.
Can you share a brief story about a time you had a positive impact on a patient, population, or community in your role as a pharmacist?
Right now I’m building a field medical science liaisons team to educate health care professionals and the community. We are hoping to educate about vaccines in general, as well as the safe and effective use of our COVID-19 vaccine product.
What do you do in your free time?
In my free time, I serve as Recording Secretary and Co-Chair of the Technology Committee for Delta Sigma Theta, Sorority, Inc. and as Vice President of Marketing for the Junior League of Philadelphia. I am also a board member of Vetri Community Partnership, The Brodsky Center Advisory Board (Pennsylvania Academy of Fine Arts), UNC Pharmacy Alumni Association, and UNC’s Alumni Committee on Racial and Ethnic Diversity (ACRED).
Meet alum Patrick Brown, Pharm.D., Senior Program Manager at the North Carolina Division of Public Health

In this alum spotlight, we chat with Patrick Brown, Pharm.D. (Class of ’13), Senior Program Manager at the North Carolina Division of Public Health.
Please describe your novel practice setting. What makes your career path unique?
I joined the North Carolina Department of Health and Human Services on January 19 as a Senior Program Manager in the Division of Public Health. Right now, I am exclusively focused on COVID-19 response, specifically working to support our COVID-19 response efforts in long-term care facilities and vaccine rollout into those facilities, and I am also the operational lead for North Carolina’s for community pharmacy vaccine rollout.
What led you to this career path? What steps did you take?
I came into pharmacy school thinking I wanted to be an independent pharmacy owner. But, when I was getting closer to graduation, I realized I wanted to get a broader perspective of pharmacy before I made any major career decisions, so I pursued a community pharmacy residency. My residency really made me realize that I like the bigger picture stuff more than the day-to-day of pharmacy operations. So I came back to UNC after graduation to pursue a fellowship where I got to continue to explore that. From there, I joined Mutual Drug where I was lucky to spend almost five years supporting independent pharmacies in a variety of roles. From there, I started to really think that maybe I would be interested in broadening my horizons. This opportunity came up at the NC Division of Public Health and I decided to make the jump and move into more of a public health role.
What does a typical workday look like for you?
Right now, most days are meeting heavy, with a heavy focus on coordinating our vaccine rollout. It’s been an all-hands-on deck approach at the state, and there are a lot of moving pieces to say the least. Most of my day-to-day is working to connect the dots between all of the different teams working vaccine and Long Term Care response at the state to our frontline providers.
Describe the most exciting or rewarding aspect of your (novel) practice role?
Right now, it’s being a part of the vaccine rollout. It’s a once in a century moment. As overwhelming and tiresome as it can be, it’s pretty incredible to be helping to coordinate this effort.
Describe the most challenging aspect of your role?
It’s all of the moving pieces. This is a monumental undertaking trying to rollout vaccines to the 10+ million North Carolinians. So it’s about the speed at which we have to move, especially since I joined after the rollout had already started.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
There are a surprising number of pharmacists involved in this effort. If pharmacists are interested in public health, I think the biggest thing is to find ways to network outside of conventional pharmacy circles. Go to meetings, lectures and symposiums that aren’t just pharmacy-related, but are health care-related. The other thing is to look into jobs that don’t necessarily have ‘pharmacist’ in the title. Throw your name in the hat. The hiring manager may have never considered a pharmacist for a role only for it to prove to be a perfect fit. That’s how I found my way to this current position.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
There is an MPH dual degree program at the UNC Eshelman School of Pharmacy. For students who are really interested in public health, that would be a good way to broaden your horizon. And always keep an eye out for internships or fellowships and lean on the student affairs office to connect with others in similar roles. And certainly find ways to network with Public Health students at Gillings.
What general advice would you give to a high school or college student who is interested in pursuing a pharmacy career?
High school or college students need to understand that pharmacy is more than just working at the drug store on every corner. Those are great jobs, but those are not the only jobs for pharmacists. Come into pharmacy school with an open mind about the profession. And be ready to blaze your own trail.
Can you share a brief story about a time you had a positive impact on a patient, population, or community in your role as a pharmacist?
In my current role, the most impactful thing we are doing right now is trying to help long-term care facilities gain access to COVID-19 vaccines. It’s been especially rewarding to be able to connect long-term care facilities and group homes who have not been able to get their residents and staff vaccinated to pharmacists in their communities that can help. The relief in someone’s voice when they hear that a vaccine event has been scheduled for them can be quite powerful. We still have a long way to go, but it’s nice to be contributing towards the effort to get back to normal.
Meet alumna Sarah Cobb, Director of Safety Project Leadership and Strategic Solutions at IQVIA

In this alum spotlight, we chat with Sarah Cobb, BSPharm (Class of ’84), Director of Safety Project Leadership and Strategic Solutions at IQVIA. In this role, Cobb oversees global pharmacovigilance projects to ensure patient safety.
Please describe your novel practice setting. What makes your career path unique?
As a Safety Project Director, I direct and oversee the service delivery excellence of a range of regional and global pharmacovigilance projects covering single and multiple lifecycle safety functions. IQVIA is a human data sciences company. We focus on advanced analytics and technology that drive healthcare forward. My career path began as a community pharmacist and includes several different pharmacy-related positions throughout my journey.
What led you to this career path? What steps did you take?
My non-traditional pharmacy career evolved over time. When I was floundering at the beginning of my sophomore year in college, my advisor gave me a career test and pharmacy consistently appeared at the top. Pharmacy combines my love of people, math and analytics. Since I love people, I wanted to be in a position to help people. After shadowing my hometown pharmacist and working as a volunteer in a pharmacy during the summer, I concluded I wanted to be a community pharmacist. While attending pharmacy school, I loved everything about pharmacy! I participated in career day my 4/5 year and found a job as a summer intern with Peoples Drug in Virginia. The summer internship gave me the opportunity to build relationships throughout the organization, leading to a full-time position upon graduation. I sincerely enjoyed my first job as a community pharmacist! I learned how to be a real pharmacist while working at Peoples Drug. While working as a community pharmacist, I also worked in a hospital pharmacy some evenings and weekends to maintain my hospital pharmacy knowledge. After a couple of years, I decided to move closer to Chapel Hill as I missed going to Tarheel basketball and football games. I was offered a job at Wake Med and moved to Raleigh. After approximately two years, I was offered a position at a small startup company, Biomedical Homecare, which was a unique pharmacy experience. After marrying a community pharmacist, life continued to change. We moved to the Sandhills area and I worked for an independent pharmacy. One day a friend, sales representative, visited our pharmacy and encouraged me to consider being a pharmaceutical sales representative. My next endeavor was working as a professional sales representative for Merck. After my husband and I had our first baby and the overnight sales traveling expanded, I resigned and worked in a hospital pharmacy. Next, I was blessed to have the opportunity to work for GlaxoSmithKline, beginning in Pharmacovigilance. I had several positions within the Company, including helping to build a world-class call center. After two major mergers/acquisitions and over 18 years, I was sitting in my office and I thought about how I wanted to return to healthcare directly helping patients and understanding the value of electronic health records. Duke Health hired me as their EPIC Clinical Inpatient Training Manager. What grand experience being part of such a huge project, all working for a common goal. Once the EPIC implementation was completed, I wanted my next challenge to include pharmacovigilance and data analytics as I envisioned the benefit of maximizing data analytics to enhance end-to-end pharmacovigilance. I started with Quintiles and after a couple of years, Quintiles and IMS Health became IQVIA, a human data sciences company. Currently, I am a Safety Project Director. When people ask me what I do, I reply: “I am a non-traditional pharmacist.”
What does a typical workday look like for you?
Working for a global company is quite different than working a 9 to 5 job. Additionally, the pharmacovigilance clock never stops. We are continuously monitoring global safety projects, ensuring patient safety. I begin my work day about 6:30 or 7 a.m. solving problems, creating new processes and ensuring the safety of our clients’ products. Due to different time zones, some meetings may take place late at night. That’s rare, however a reality. Typically, I try to stop working by 6 p.m. Sometimes I will return to my office after dinner to check emails as my collaegues on the other side of the world are beginning their day.
Describe the most exciting or rewarding aspect of your (novel) practice role?
The people! I enjoy interacting with people all over the world. The majority of my day is spent talking to people in the Asia-Pacific and European areas which is rewarding. I have learned a great deal about different cultures and traditions as well as global holidays. I meet new people and learn new things while having the privilege to lead patient safety teams and collaborate with pharmaceutical and clinical research industry colleagues.
On another note, I recently became a certified pharmacy-based vaccine immunizer to help administer COVID vaccines and other vaccines in the future. The most rewarding experience in my pharmacy career has been observing how appreciative people have been when receiving their COVID vaccines.
Describe the most challenging aspect of your role?
The most challenging aspect of being a Safety Project Director is the safety clock never stops (24/7), especially during global inspections and audits.
How can someone learn more about this unique practice setting and the career opportunities it presents for pharmacists?
I always remind students to maximize their network inside and outside of the Pharmacy school. Talk to leaders within the Pharmacy school and pharmaceutical industry. A good way to get a foot in the door is by doing a summer internship or volunteering. Several pharmacy students from UNC have worked at IQVIA for that purpose.
What advice would you give to a current student pharmacist who is interested in pursuing a similar type of practice role in the future?
I would highly encourage students to become a traditional community or hospital pharmacist first unless they are on a specific career track leading them to be a non-traditional pharmacist. If they are not 100% sure what they want to do, I recommend learning how to be a community pharmacist while treating patients. As a community pharmacist, they will learn how to dispense medications, identify drug interactions, build relationships with patients and colleagues while creating the foundation of their pharmacy career. Community and hospital pharmacy experiences were the foundation of my non-traditional pharmacist career.
What general advice would you give to a high school or college student who is interested in pursuing a pharmacy career?
I would encourage the student to research pharmacy careers and learn as much about pharmacy as possible via networking or volunteering. Collaborate with pharmacists in various roles. Build a network and attend career days. A big advantage would be to talk to their advisor(s) and shadow some pharmacists working in different pharmacy settings. My husband and I have participated in numerous high school career days as we love to talk with students about different pharmacy-related career opportunities. I would recommend researching pharmacy via the internet and learning more about the different pharmacy schools. Take the time to explore options.
Can you share a brief story about a time you had a positive impact on a patient, population, or community in your role as a pharmacist?
Wow, there have been so many! During my community and hospital pharmacy ventures, I worked for a startup home healthcare company. As a pharmacist, I was on-call certain weekends and carried a beeper. One weekend, I was beeped. We had a cancer patient who was out of his saline syringes. I needed to take some syringes to him as soon as possible. He lived somewhere between the Sandhills and Raleigh. Since it was late in the day, my husband rode with me. When we arrived, the setting was like something you would see in a movie. He lived down a long dirt road in a little old house. I walked up to the front door with the box of syringes and knocked on the door. Several family members invited me inside and were so appreciative to see the syringes. The patient was lying in a hospital bed in an extremely small family room just inside of the front door. When I walked out to my car, tears were rolling down my face. I will never forget that poor little man’s name and his family.
Download our Pharmacy Career Guide to learn more about pharmacy careers.
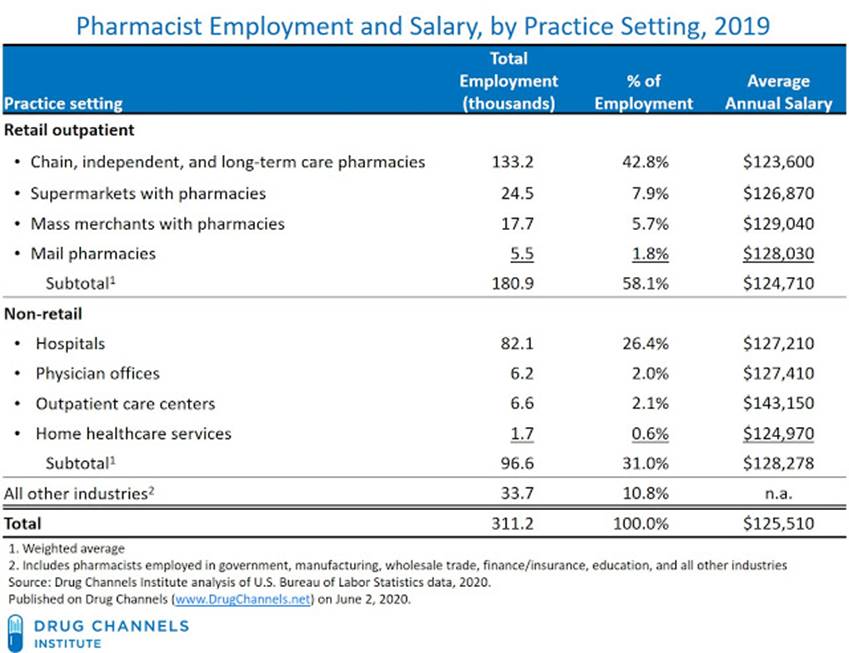
Pharmacy Salaries