January 18, 2024
Four years since SARS-CoV-2 first spread across the U.S., there are still tens of thousands of new weekly COVID hospitalizations, underscoring the need for more effective means to prevent these infection-induced hospitalizations. Sam Lai, Ph.D., professor in the Division of Pharmacoengineering and Molecular Pharmaceutics at the UNC Eshelman School of Pharmacy, is advancing an inhalable antibody treatment that not only works against all SARS variants but can be dosed with at-home convenience rather than the traditional means of systemic infusion.
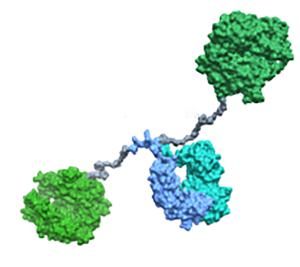
Lai’s research spans the interface of immunology and engineering, with a particular emphasis on developing novel bioactive molecules that can better reinforce mucosal health. A decade ago, his lab discovered that antibody molecules can be tuned to interact with mucins, the key building block of mucus that gives it its sticky texture. This allows antibodies to bind bacteria or virus at mucosal surfaces, trap them in mucus and block the spread of the infection.
“My lab used this knowledge to develop different interventions against viruses,” he said. “When COVID-19 happened, we recognized the challenge that the virus is very likely to mutate quickly and escape from conventional antibody therapies. So, we wanted to approach it differently than most labs were doing at the time.”
This led the team, including postdocs Karthik Tiruthani, Ph.D., and Carlos Cruz-Teran, Ph.D., to deliberately swap the virus binding domains of an antibody with the portion of the ACE2 receptor that SARS-CoV-2 binds to infect cells. The end result is a molecule that is not at risk of viral escape, since any virus that evades this novel molecule would by definition not bind target cells. The molecule is effective not just against SARS-CoV-2, but any virus that targets the ACE2 receptor – an important pandemic preparedness consideration.
In addition to the novel design of the molecule, the team also worked extensively on the delivery strategy that allows this pan-SARS treatment to be given in a mist form that can be readily used by patients of all ages.
“Most of these respiratory infections are in the lung, so it’s much more efficient to deliver our molecule by inhalation versus injecting into the blood,” Lai said. Using a hand-held unit, patients breathe in this mist for a few minutes a day from home, without having to go into a health care facility.
The work, which will be published in the journal Bioengineering and Translational Medicine, demonstrates their molecule can effectively trap SARS-CoV-2 in fresh human airway mucus, and effectively suppress viral load in hamsters.
Reflecting both the existing need for safe and effective pan-SARS intervention, and the promise of Lai’s inhaled immunotherapy approach, the U.S. Army Medical Research and Development Command has committed $5.7M to advance his lab’s pan-SARS molecule into clinical trial. The team expects to be ready to start phase one of the clinical trial in early 2025.
Lai’s pioneering work on muco-trapping antibodies led to the formation of several startups, including Inhalon Biopharma, a clinical stage startup focused on treating acute respiratory infections. Inhalon has licensed the pan-SARS molecule and is the commercial entity leading the clinical development efforts. This research was earlier supported by a North Carolina Collaboratory grant.
Latest News

RASP poster presentations capture student research

Delesha Carpenter promoted to full professor


