July 31, 2020
Researchers from the UNC Eshelman School of Pharmacy, the UNC School of Medicine, and the University of Florida have teamed up to study the effect of using genetic information to guide treatment after an angioplasty heart procedure on preventing heart attacks and strokes.
The group recently received a $3.5 million grant from the National Heart, Lung and Blood Institute (NHLBI) to pursue their work.
Blood clots leading to heart attack or stroke are one of the most common complications following an angioplasty, also known as a percutaneous coronary intervention. In the procedure, doctors place a stent to open blocked or narrowing arteries in the heart. Afterward, patients are prescribed aspirin and other blood thinning medications to prevent clots.
About 30 percent of patients in the U.S. carry a gene variant that reduces the effectiveness of the blood thinning drug clopidogrel. Genetic testing can help prescribers determine the right drug for angioplasty patients to reduce the risk of blood clots and avoid prescribing an ineffective medication.
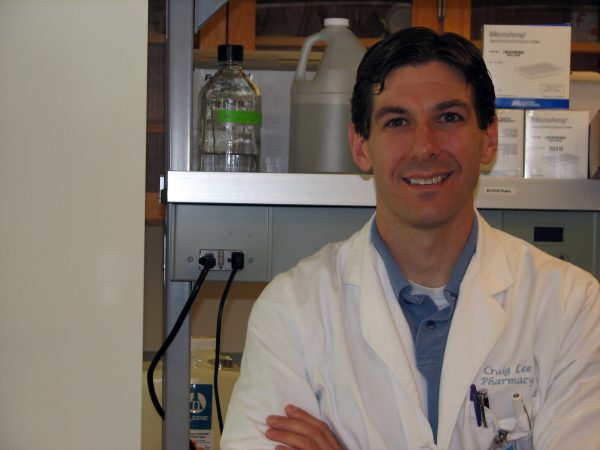
Craig Lee, Pharm.D., Ph.D., associate professor in the Division of Pharmacotherapy and Experimental Therapeutics at the UNC Eshelman School of Pharmacy, and Larisa Cavallari, Pharm.D., associate professor of pharmacotherapy and translational research at the University of Florida College of Pharmacy, will serve as principal investigators on the grant. Joseph Rossi, M.D., associate professor at the UNC School of Medicine and director of the UNC Cardiac Catheterization laboratory, will serve as a co-investigator on the grant.
“If we can establish the key factors influencing outcomes with these genotype-guided therapies, then we have a real opportunity to further help prevent death, heart attack, and stroke after angioplasty,” Cavallari said.
More than 6,000 angioplasty patients from across North Carolina and Florida will be included in the NHLBI study. UNC and UF researchers will work to study outcomes over the course of 12 months to better understand who to genotype, what to include on a testing panel, how patient-specific factors influence therapies and how to change medications for angioplasty patients based on the results.
“We have previously demonstrated the feasibility and clinical benefits of using a patient’s genetic information to guide antiplatelet medication prescribing after a stent procedure,” Lee said. “This project will enable us to determine what additional factors influence patient outcomes and ultimately optimize strategies for physicians and pharmacists to individualize antiplatelet therapy prescribing decisions.”
Latest News

Dean Angela Kashuba receives Carolina Alumni Faculty Service Award

RASP poster presentations capture student research


